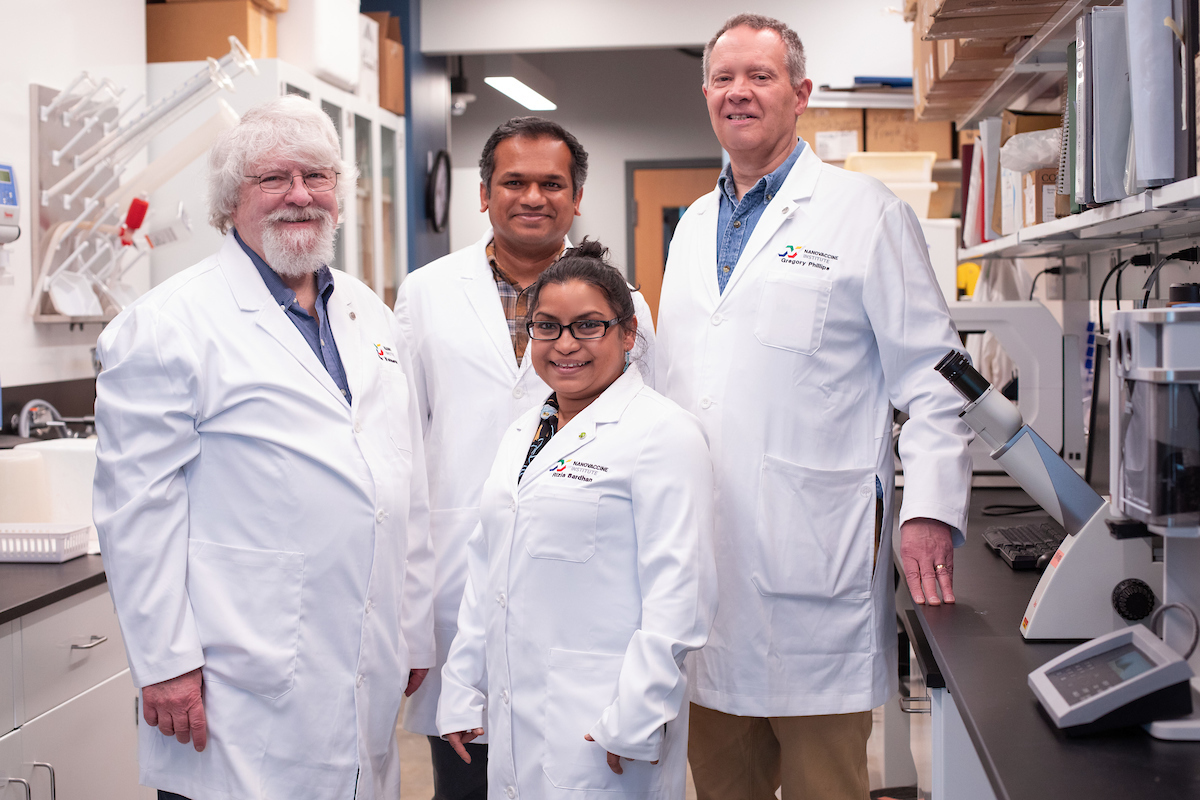
Iowa State researchers, left to right, Michael Wannemuehler, Saji Uthaman, Rizia Bardhan and Gregory Phillips are designing and testing nanoparticles to treat inflammatory bowel diseases. Larger photo. Photo by Christopher Gannon/Iowa State University.
AMES, Iowa – Drug-delivering nanoparticles could improve treatments for inflammatory bowel diseases that affect the quality of life of more than 3 million Americans, Iowa State University researchers say.
While there are treatments today, they tend to be short-term, with patients developing resistance to drugs and relapsing into inflammation and symptoms of diarrhea, severe stomach aches, bloody stools and extreme fatigue.
What could help?
Enter the tiny, spherical micelle.
Micelles are self-assembling wonders just 250 billionths of a meter in diameter. The spheres are created when chains of lipid molecules are exposed to water, causing the hydrophilic, water-loving heads of the molecules to form an exterior shell and the water-hating, hydrophobic tails to turn to the inside of the shell.
Rizia Bardhan, an associate professor of chemical and biological engineering at Iowa State University, and other Iowa State researchers say the smart design of micelles could be just the treatment for bowel conditions such as Chron’s disease and ulcerative colitis.
The U.S. Department of Defense’s Congressionally Directed Medical Research Programs are supporting the researchers’ micelle work with a two-year, $306,000 grant.
Bardhan, who has expertise in using nanoparticles for medical applications, is leading the project. Additional team members include:
- Michael Wannemuehler, with expertise in inflammatory bowel diseases, a professor of veterinary microbiology and preventive medicine
- Gregory Phillips, with expertise in gut microbiomes, also a professor of veterinary microbiology and preventive medicine
- And Saji Uthaman, with expertise in the synthesis of micelles, a research scientist in chemical and biological engineering
- All are affiliated with the Nanovaccine Institute based at Iowa State.
Hitting the target, enabling gut health
Bardhan said the researchers will be using hyaluronic acid, a natural biopolymer already used in human medicine, to make therapeutic micelles that can be loaded with a drug that inhibits an immune protein known as STING. Recent studies indicate that activation of the protein can worsen the symptoms of inflammatory bowel diseases.
The U.S. Food and Drug Administration has not approved any drugs that inhibit the STING protein. The researchers say this is, in part, because inhibiting drugs have been tested, but they’re quickly cleared from the body and are difficult to target, so they often fail to reach the inflammation.
“It’s important to target the drug to the inflamed colon,” Bardhan said. “We don’t want it to nonspecifically accumulate in other organs.”
The researchers’ micelles, however, can be loaded with the inhibitor, keeping it in the body for hours. The hyaluronic acid also naturally targets cell receptors expressed in the inflamed colon, bringing the micelles to the inflammation site. Once there, a trigger releases the drug payload.
“The near-term impact of our project will allow a safe micellar formulation of a potent drug for immediate reduction in (inflammatory bowel disease) symptoms with low doses and minimal side effects, and enable a healthy gut environment,” according to Bardhan and Wannemuehler.
Over the long term, the researchers say their STING-inhibiting micelles could impact the design of drug delivery for other conditions linked to STING increases, such as Parkinson’s disease. They said the micelles could also be turned into pills for easy and convenient use.
“The biggest challenge with these inflammatory bowel diseases is there’s no cure,” Bardhan said. “Many patients acquire resistance to existing treatments and those treatments don’t work anymore.”
These new, smartly designed and purpose-built nanoparticles, the researchers said, could be the transformative agents doctors and patients are looking for.
